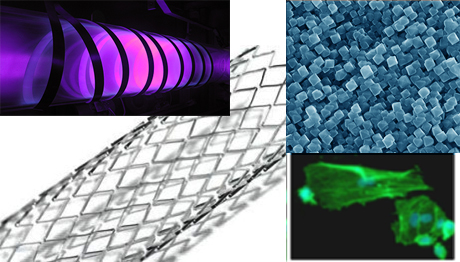
Advanced hemocompatible surfaces of vascular stents (L7-7566)
Project leader: Dr Ita Junkar (Jozef Stefan Institute)
The project will focus on improving surface properties of stents made of titanium. Although titanium alloys are extensively used for stent application they still lack of desired biological response, mostly due to restenosis. Restenosis presents a huge problem on all stent surfaces. It occurs in more than 33% of the cases, with higher possibilities in patients with high risk factors, such as diabetes. The stents can be divided in bare metal stents (BMS) and drug-eluting stents (DES). With DES the problems of allergenic reactions as well as risks of restenosis were lowered, as DES release anti cell-proliferative, immunosuppressive or anti-thrombogenic drugs which inhibit proliferation of smooth muscle cells and reduces thrombus formation. However it was shown that DES also inhibits normal endothelium growth which potentially leads to thrombosis. The probability of death by cardiac infarction in the period of 6 months to 3 years after implementation of DES was 32% higher than on BMS [Lagerqvist B. et al., New England Journal of Medicine 2007, 356, 1009-1019]. Therefore in the last few years adverse clinical data linking DES usage to arterial thrombosis had led to a large decrease in sales. Furthermore, companies are seeking to develop novel stents, while so far the improvements on DES are merely incremental. Innovations are done mostly on the polymer coatings, stent platforms and on drug components. Moreover DES are almost three times more expensive compared to BMS.
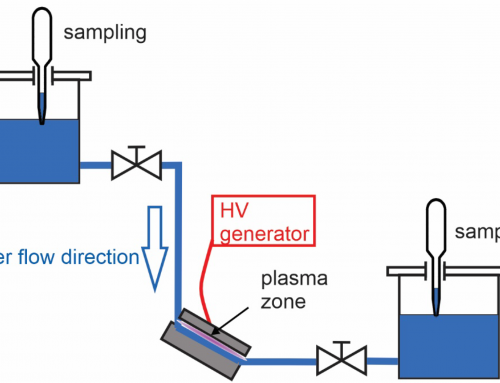
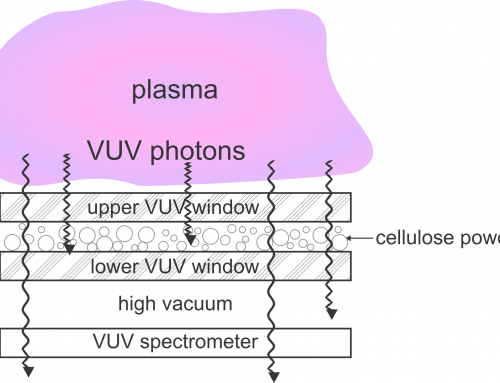
Therefore the main goal of the proposed project is to provide advanced stent surfaces which will lower the risk of restenosis as well as thrombosis, without the need to use coatings. This will be achieved by electrochemical anodization and plasma treatment technique. By electrochemical anodization we will form self-assembled layers of vertically oriented TiO2 nanotubes with defined diameters between 15 and 100 nm. These surfaces will be further treated by highly reactive plasma in order to increase oxygen content on the surface and to remove surface residues obtained from electrochemical anodization. As sterilization is the final surface treatment step, which should be considered before implementation, systematic studies on effects of commons sterilization techniques on surface properties as well as on the biological response will be conducted. Biomimetic surfaces are increasingly recognized for their surface features as they were shown to highly influence on tissue acceptance and cell survival. However effects of surface chemistry and wettability should not be neglected as synergistic effects can be achieved by fine tuning morphological and chemical features. Our previous results (obtained in the frame of ARRS project »Preparation of hemocompatible polymeric surfaces for biomedical applications«, Z3-4261, 2011 to 2013) on plasma treatment of vascular grafts made of polymers indeed showed significant reduction in platelet adhesion and activation, while enhanced proliferation of endothelial cells due to nanostructuring and functionalizing the surface by plasma (formation of oxygen functional groups). As titanium surface cannot be nanostructured by plasma, electrochemical anodization will be employed and surface chemistry will be appropriately altered by high reactive plasma. In tight collaboration with experts in material engineering, surface sciences, plasma physics and medicine we will be able to accomplish desired biological response on titanium surface. Therefore we aim to develop new generation stents by combining the two novel techniques (electrochemical anodization and plasma treatment). By this we believe to fabricate appropriate nanostructure as well as surface chemistry which will reduce smooth muscle cell growth, prevent platelet adhesion while promoting proliferation of endothelial cells.